The arteriolar injury in “resistant” hypertension (with figures)
(BMJ website at http://www.bmj.com/content/358/bmj.j3984/rr)
Uncontrolled hypertension “resistant” to three, concurrent, antihypertensive drugs is an alarming diagnosis with significant, subsequent cardiovascular morbidity (Sinnott, 2017). Treating the condition as a syndrome may suit contemporary pharmacological approaches but, in many cases, there is an historical, renal arteriolar injury that may better define the condition (Moritz & Oldt, 1937). Moritz & Oldt reported arteriolar stenosis in kidney (1A-D), spleen (2A-D), pancreas and adrenal in hypertensive patients of both sexes, across the age range with an increasing incidence with advancing age. Their central question was; is this injury a cause or a consequence of hypertension ?
1A) 1B)
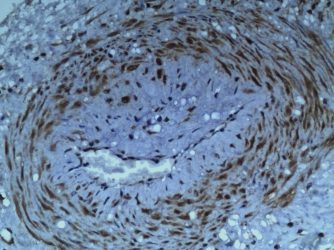
Fig.1 injured uterine and renal arterioles stained with anti S100(Fig.1A,C), HE (1B,D) and anti-P2X3 (1E,F). The pattern of perivascular hyalinisatiin in the uterus (1A) is different from kidney (1D) and corresponds to site of the “halo of hyalinisation” in non-pregnant, painful uterus (1A). Compare same in kidney (1C-D).
We find that injuries to vasomotor nerves in renal (and other visceral) arterioles leads to release of cytokines, regeneration of injured nerves with concurrent hyperplasia of the denervated-vessel walls (1A&D). Injured arterioles express purinergic, P2X3 ”stretch” receptors (1E&F) and, are susceptible to hyaline and fibrinoid changes. Salt, sugar, stress, smoking, and straining at stool may all contribute to hypertension associated with these vasomotor injuries. Subsequent narrowing of renal arterioles also plays into the development of “resistant” hypertension through classical, Goldblatt mechanisms associated with relative ischaemia. At a certain threshold, the arteriolar injury may be both a “cause and consequence” of hypertension producing a downward spiral of deteriorating consequences that ends as the syndrome of resistant hypertension. Preventing the initial injuries by amending lifestyle choices to avoid peaks of renal arteriolar blood pressure that damage injured arterioles, may further reduce the rate of resistant hypertension ?
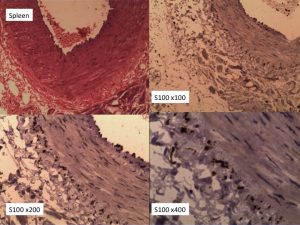
2A 2B
Fig. 2 Injured splenic arterioles with concentric layers of perivascular reinnervation at x100, x200 and x400. The injured arteriolar wall shows evidence of medial and intimal hyperplasia. Both features arise from injuries to vasomotor nerves that release a cocktail of cytokines and growth factors that act on denervated arteriolar walls.